Section
5
Assessing Adiposity
Anthropometry
Anthropometry is the study of human body measurements that provides information on body size and dimensions.
Anthropometry is composed of physical measurements that include recumbent length (lying down length) or stature (standing height), weight, and regional dimensions, including circumference measurements, skinfold thicknesses, bone breadths, and bone lengths. Methods that are used to assess adiposity include recumbent length/stature and weight, skinfolds, and circumferences. In the context of a research study, assessors conduct these measurements in duplicate or triplicate, ensuring (at least) two measurements are within a pre-specified allowable difference from one another. The maximum allowable difference between repeated measurements will vary by method and should be specified in the study manual of procedures or operations. The average of the two closest measurements will be used in the analyses. In addition, all equipment should be calibrated according to the study manual of procedures or operations and before conducting measurements each day to ensure accuracy.53,54
Length/Stature and Weight
Recumbent length/stature and weight are the most common measurements used to assess weight status and monitor growth. These measurements are often used to calculate indices that can be used to define obesity across all ages, from infancy through adulthood.
Recumbent length is measured in infants and children from birth to 24 months using an infant length board. The board is placed on a level and hard surface. Research staff place the infant flat on the center line of the board facing upwards with eyes looking straight up and spine straight. The crown of the head is held in position against the headboard and a second staff person straightens the infants’ legs by gently placing hands on shins and knees and then moving the footboard so that soles are flat against it. The value of the measurement is recorded to the nearest 0.1 cm (Figure 5).
Figure 5: Recumbent Length Measurement in Infants
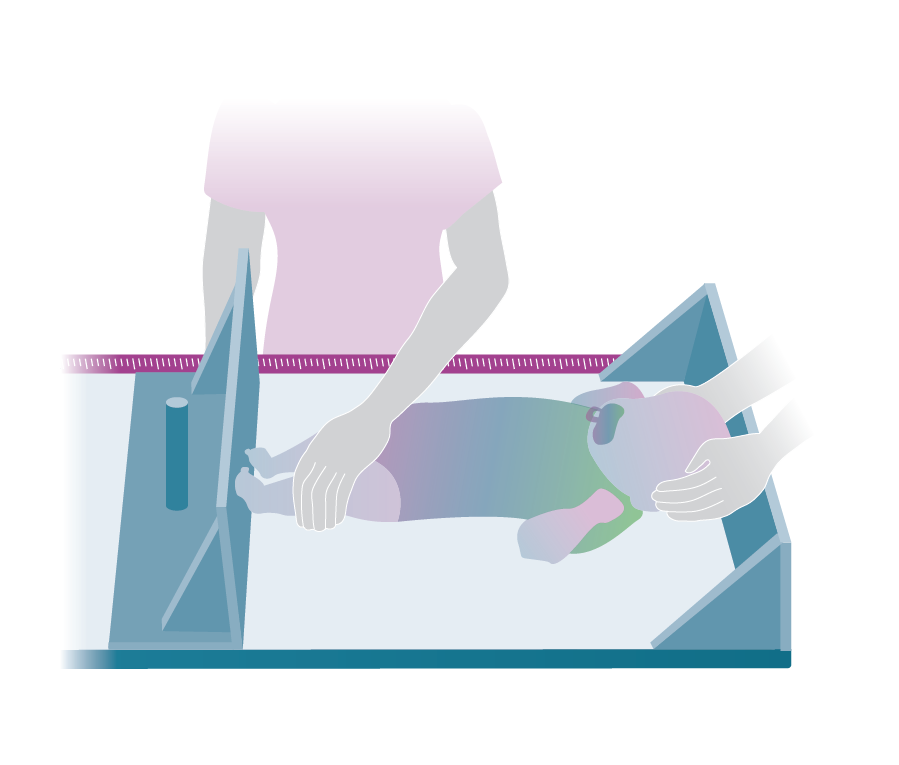
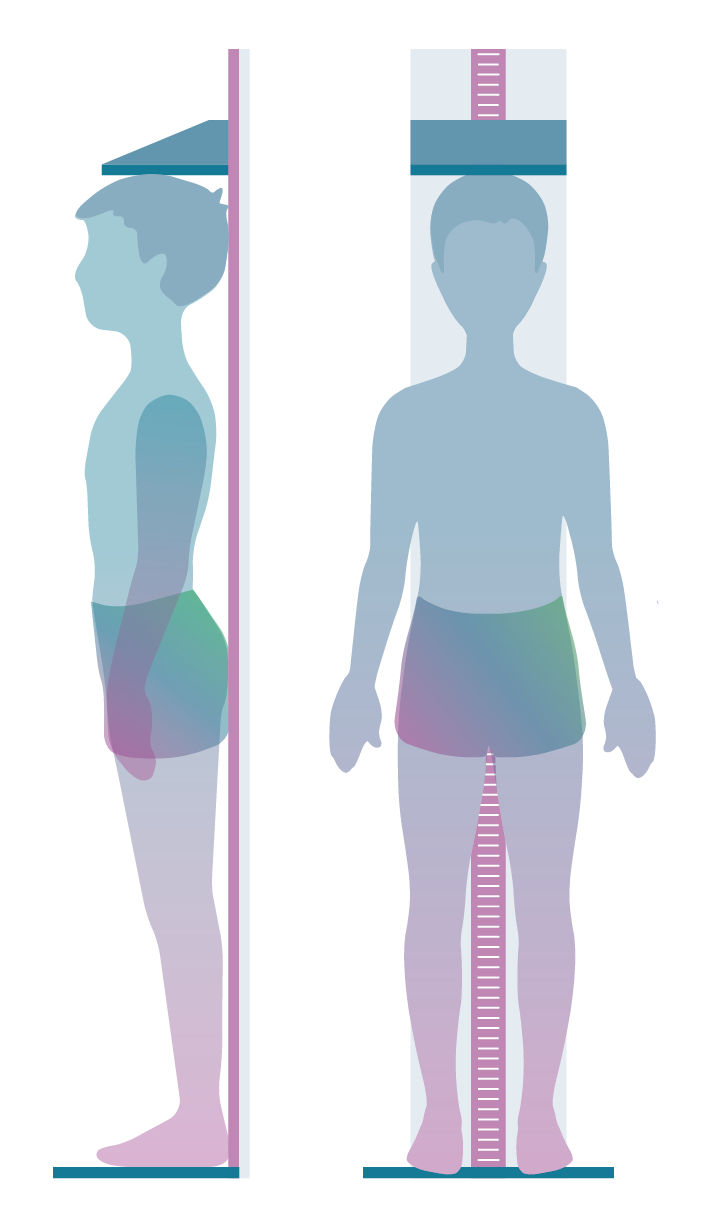
Figure 6: Stature or Standing Height Measurement in Children
Stature is measured using a stadiometer for children aged 24 months and older. With shoes removed, the child stands erect with feet positioned on the floor board of the stadiometer, arms by sides (palms facing legs), and back vertical to the backboard of the stadiometer so that the heels, buttocks, and back of head make contact with the back board (Figure 6). Children with severe obesity may not be able to have all three body parts touching the back board while standing straight. The head is positioned in the Frankfort horizontal plane. The measurement bar is lowered to contact the skull (hair should be flat with no accessories where possible) as the participant is asked to take a deep breath in. At the end of inspiration, the value of the measurement is recorded to the nearest 0.1 cm. If a child has braids or hair accessories that cannot be removed, a height adjustment ruler is used to measure the hair piece. Subtracting the height of the braid or accessory from the measured height produces an adjusted height value that better reflects the child’s actual height. A wall-mounted stadiometer with a fixed heel plate is recommended for greater reliability. Height bars attached to scales or wall-mounted tape measures are not appropriate for accurate height measurements. A certified calibrating rod should be used to calibrate the stadiometer for quality control before conducting measurements each day.
Children who have conditions that do not allow them to stand erect (e.g., cerebral palsy) can have their height estimated from surrogate measures including upper arm length, ulna length, forearm length, knee height, and lower leg (tibial) length. Measurement of tibial length does not require specialized equipment and is not impacted by knee and ankle contractures. However, whatever surrogate measure is selected, training of observers is required to ensure reliable and accurate results.55
Body weight is measured using a scale. For infants, an electronic pediatric scale is recommended, and the scale should be placed on a level and hard surface. Staff should confirm that the scale is tared (reads zero when no one is on the scale) before use. Wearing only a dry diaper, the infant is placed on the middle of the scale and weight is recorded. Children who can stand upright unassisted stand on the center of a floor scale with weight equally balanced on both feet. During the measurement, they wear minimal or light clothing and no shoes. The preferred equipment to assess weight is an electronic or beam balance scale that is properly calibrated to the nearest 0.1 kg according to the manufacturer’s directions. When the child is standing motionless, the value of the measurement is recorded to the nearest 0.1 kg. Spring balance scales, such as bathroom scales, are not sufficiently accurate. Scales also must be able to measure the range of weights, including extremes, in the sample of children under evaluation. For quality control, all scales should be calibrated daily before measurement using certified weights of varying masses across the range of subject weights being measured. It is important to note that a scale may calibrate (be accurate) at lower weight increments but begin to deviate (be inaccurate) at higher weights. For more information about which types of scales are needed, see the following resource:
Additional Resource
Estimates of Body Fat, Interpretation, and Limitations
Body mass index (BMI) is calculated from weight and height as weight per height,2 expressed in kilograms per meter squared, and is a commonly used index used to assess weight status and define obesity among adults and children aged 2 years and older. Although BMI does not measure body fat, it is highly correlated with total body fat at high levels, and thus values above a specific cut point are used to define obesity or excess adiposity.56,57 An online BMI percentile calculator for Child and Teen provides BMI and the corresponding BMI-for-age and sex percentile based on the CDC growth charts. Similarly, weight for length, expressed as kilograms per meter, is a commonly used index of weight status and of fatness in infants and children younger than age 2 years as a comparison to sex-specific weight-for-length percentiles. As described in Section 2: Defining Overweight and Obesity in Children, an expert committee comprised of representatives from 15 professional organizations defined overweight in children aged 2 years and older as the 85th to 95th percentile of BMI for age and sex, and obesity as BMI ≥ 95th percentile or an absolute BMI ≥30 kg/m2, whichever is lower based on age and sex using the reference population from the 2000 CDC growth charts.4 In addition, CDC recommends that for children birth to age 2, weight-for-length at or above the 97.7th percentile (+2 z-scores) of the sex-specific WHO growth charts be used as a cutoff.5 More recently, the American Heart Association recommended that severe obesity in children aged 2 years and older be defined as having a BMI ≥120% of the 95th age- and sex-specific percentile or an absolute BMI ≥35 kg/m2, whichever BMI value is lower.6
Weight and height/recumbent length are relatively simple and inexpensive to collect and widely used to calculate indices (BMI and weight-for-length) that define obesity or excess weight in childhood. However, these indices have limitations for use in research and thoughtfulness must be used in their interpretation:
- BMI, as well as weight-for-length, is a measurement of body mass (the sum of both FM and FFM) and does not provide quantitative information on body composition (i.e., amount of FM versus and FFM) or the distribution of FM and FFM.
- BMI has poor ability to discriminate between FM and FFM because these two components are highly correlated (e.g., having a higher FM is associated with having higher FFM).
- In most children, BMI does not provide a valid index of fatness.58 In prepubertal children aged 6 to 12 years, BMI accounted for only 54% and 69% of the variability in percentage of body fat in girls and boys, respectively. The average percent error predicting body fat ranged from 20.3% in girls to 22.5% in boys.59
- BMI may overestimate or underestimate body fatness, particularly in the overweight range (BMI 85-95th percentile, and also varies widely by race/ethnicity. For example, about 50% of non-Hispanic white girls aged 8–19 years in the overweight category have excess body fat by DXA, but among non-Hispanic black girls, fewer than 25% have excess body fat.29
- Studies that used BMI to identify children with overweight and obesity based on percentage of body fat have found high specificity (95 to 100%), but low sensitivity (36 to 66%) for this system of classification.60,61 This suggests a tendency to misclassify individuals as having overweight or obesity when they do not have excess body fat.
The current version of the CDC growth charts are not intended to be used for BMI z-scores and percentiles above the 97th percentile because changes in extreme values are compressed into a narrow range of associated z-scores or percentiles that do not reflect meaningful changes.62 CDC is undertaking an effort to resolve this and updated guidance will be found on the CDC Growth Charts webpage.
- Interventions that affect body fat and/or lean mass but use BMI as the outcome measure may fail to detect changes in BMI.63-66 For example, higher levels of physical fitness are associated with increases in FFM and decreases in FM. If changes in FFM and FM both occur and are equal, BMI may not change. Therefore, the use of BMI as an outcome measure in fitness interventions designed to affect fat and/or fat-free mass has the potential to miss positive effects of interventions.67 Similarly FM and FFM, not necessarily BMI, are associated with cardiometabolic risk, and studies using BMI may fail to detect associations with indices of health-related outcomes, such as biochemical markers of cardiometabolic risk.68
The use of BMI in intervention studies as an outcome measure to establish efficacy of dietary and/or physical activity interventions that are intended to reduce adiposity has limitations. That is, some persons with a low BMI may have a relatively high percent body fat (because, for example, they have low muscle mass), while others with a high BMI can have a low body fat (because, for example, they have high muscle and bone mass). One cannot assume that small changes in BMI, or differences in BMI between individuals or subgroups of a population, completely reflect differences in body fat.
Validity and Reliability
As previously described above, BMI does not measure fat mass. Therefore, studies that examine its performance examine correlations of BMI with various other methods that do estimate fat (such as air displacement plethysmography (ADP) and dual energy X-ray absorptiometry (DXA)) and describe the degree to which the relative relationships are consistent. In infants measured at birth and again at 5 months in the Healthy Start study, fat mass by ADP was significantly associated with BMI z-score.69 For children aged 6.5–10.9 years in the pre-birth cohort Project Viva, total fat mass by DXA was highly correlated with BMI.70 For children aged 8–18 years, correlations between BMI z-score and percent fat mass by DXA were moderate to strong, with the strongest correlations for boys and girls aged 8–11.9 years old.71 For children aged 8–20 years, the correlations between BMI z-score and fat mass showed strong associations across all participants combined, and moderate associations for participants with moderate or severe obesity.62 For more information about BMI validity and reliability see the following resources:
Additional Resources
- Relation of BMI to Fat and Fat-free Mass Among Children and Adolescents
- Diagnostic Performance of Body Mass Index to Identify Obesity as Defined by Body Adiposity in Children and Adolescents: A Systematic Review and Meta-analysis
- Fat and Lean BMI Reference Curves in Children and Adolescents and Their Utility in Identifying Excess Adiposity Compared with BMI and Percentage Body Fat
Reference Data
National reference data for recumbent length for children from birth to 47 months, stature for children aged 2–19 years, weight for children from birth to 19 years, and BMI for children aged 2–19 years old are available from the NHANES 2011–2014 sample that included participants of all ages.72 These reference data are the most recent population-based reference data available for comparisons.
Accessibility, Training, and Cost
Equipment to measure recumbent length/height and weight is highly accessible, portable, and costs relatively little, although cost can vary considerably depending on the make and model of equipment. Typically, a research-grade portable scale or stadiometer costs about $300. Training is needed to standardize measurements, but this measurement process requires relatively less skill than do other methods that will be described in this guide.
Acceptability, Participant Burden, and Risk
Acceptability is high, when privacy is maintained, and burden to participants is low. The methods are noninvasive, safe, and low risk.
Summary
Recumbent length/stature and weight measurements and the indices of BMI and weight-for-length that are used as indicators of weight status and excess adiposity are simple, safe, quick, and very acceptable. The measurements attained by this method are inexpensive to collect and require less staff training and skill for accurate and consistent measurement than do other methods. These methods are thus appealing for large-scale studies. However, these indices have limitations as they are not measuring body fat, and caution must be used in their interpretation.
Skinfold Thickness
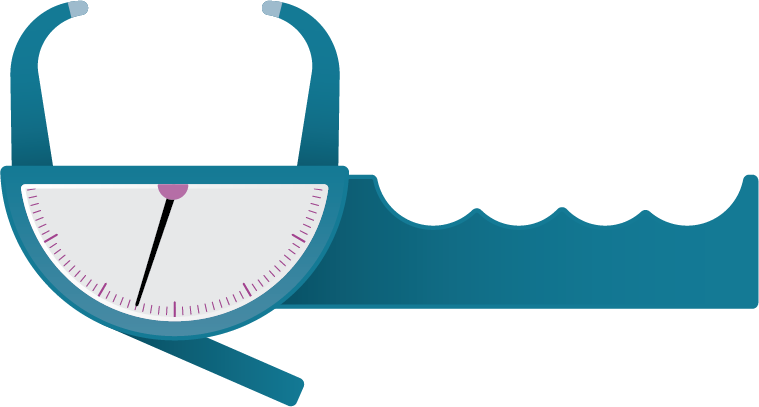
Figure 7: Skinfold Caliper
Skinfold thicknesses are measured using calipers (Figure 7) to assess the thickness of the subcutaneous fat layer. Because the subcutaneous fat layer varies in thickness across the body, measuring sites at different anatomical locations of the body can assess upper and lower body fat distribution. Skinfold thicknesses can be used across all ages, from infancy through adulthood.
Procedure
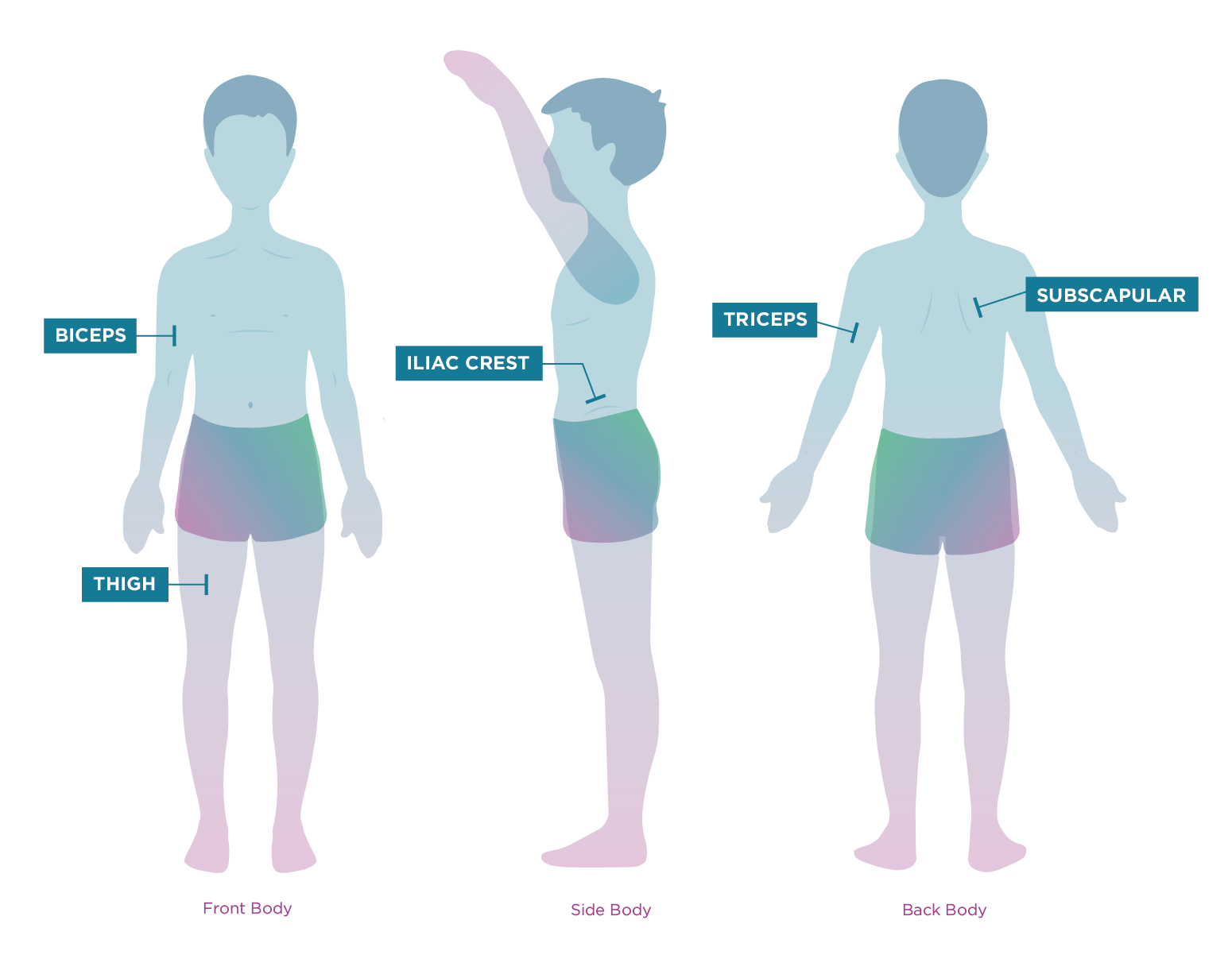
Participants should wear loose clothing and short sleeves so that the targeted area of the body can be freely accessed and measured. All measurements should be taken on dry, oil- and lotion-free bare skin. The type of caliper is important in the assessment of skinfolds. Calipers in which the pressure is built into the instrument itself (spring loaded) and is relatively constant from reading to reading and over the range of skinfold thickness studied are recommended. Spring-loaded levers provide a substantially constant, standard pressure of 10 g/mm2 over the entire operating range. Ideally, the same skinfold caliper should be used throughout a single study for all skinfold measures. Examples of spring-loaded calipers include Harpenden, Holtain, and Lange. These calipers will measure skinfold thickness of up to approximately 50 to 60 mm. The resolution is 0.2 mm units, though it may be accurately read from the scale to the nearest 0.1 mm. Most skinfolds are drawn up in a vertical line at the selected location on the body. A washable marker or cosmetic pencil can be used to mark the location of the skinfold measurement site to ensure consistency for repeating the measurement. The person taking the measurement uses his or her thumb and index finger to pinch the skin at the appropriate site and pull it away from the underlying muscle. This ensures raising only a double layer of skin and the underlying adipose tissue. The calipers are then applied 1 cm below the pinch at a right angle to the pinch, and a reading in millimeters (mm) is taken 2 to 3 seconds later or when the needle settles, to the nearest 0.1 mm. The value of the measurement is recorded to the nearest 0.01 mm. Skinfold measurements are obtained on the same side of the body, at various locations, with the participant standing, as shown in Figure 8. Newborns/infants should be lying down for each measurement.
Figure 8: Skinfold Measurement Locations
When all skinfold measurements of interest on the same person have been acquired, a second set of measurements is repeated in the same order as the first set. The skinfold calipers should be calibrated daily for correct jaw tension and gap width before measurement. A standard metal calibration block is used to ensure calibration, which is important for quality control. Calipers are calibrated to exert a constant pressure of 10 g/mm2 at all thicknesses.
Location of Measurements
The following locations may be measured depending on the study outcome of interest:
- Biceps are measured at the mid-point between the bony tip of shoulder and the elbow joint on the mid-line of the front of the arm. Pinch the skin over the biceps muscle. Newborns/infants should be placed on their back for the measurement.
- Iliac crest is measured on the mid-axillary line just above the iliac crest (top border of the hip bone) on a diagonal fold. Pinch the skinfold just above the crest at an angle and place the calipers at an angle. Newborns/infants should be placed on their side.
- Subscapular area is measured just below the lower angle of the scapula (shoulder blade) at about a 45-degree angle to the spine. Newborns/infants should be placed on their stomach for the measurement.
- Thigh is measured at the mid-way point between the inguinal crease (groin region) and proximal border of the kneecap. Mark the skin at that point and place the caliper midway between the inguinal crease and the proximal border of the kneecap. Newborns/infants should be placed on their back for the measurement.
- Triceps are measured on the back of the arm. Using a tape measure, measure distance between the acromion process (tip of shoulder) and olecranon (tip of elbow) and mark the skin at mid-way point. Acquire the skinfold measure by pinching the skinfold with thumb and index finger above the mark while placing caliper on the vertical fold at the mark, which is over the triceps muscle. Newborns/infants should be placed on their stomach for the measurement.
Estimates of Body Fat, Interpretation, and Limitations
The sum of skinfold thicknesses measured at biceps, iliac crest, subscapular, thigh, and triceps sites can be used as an estimate of overall body fat. Subscapular and iliac crest skinfold sites are located on the trunk and can be used as an estimate of central fat distribution while biceps, triceps, and thigh skinfolds are located on the limbs and can be used as an estimate of peripheral fat distribution. Percent body fat can be estimated from prediction equations that use skinfold measurements that are age- and sex-specific in adults and children. Overall, skinfold prediction of percent fat has large errors at the individual level and smaller errors at the group level. Therefore, they are not useful for characterizing an individual’s body fat but are useful when estimating and comparing group averages. The measurements require skill and well-trained staff, and it is often difficult to capture only the subcutaneous fat when conducting the measurement. In addition, it is difficult to obtain reliable measurements when different staff members take the same measurements. However, with training, high levels of reliability can be obtained.
Validity and Reliability
For newborns and infants, low correlation exists between body fat prediction estimates from skinfolds and body fat estimates by more accurate methods, including total body water (deuterium dilution technique) and MRI.73,74 The widely used Slaughter skinfold percent fat prediction equation was developed in a predominantly lean cohort three decades ago.75 When applied to a modern-day sample of children and youth aged 6–18 years, the Slaughter equation was a fairly accurate estimator of percent fat compared to DXA-calculated percent fat among children without obesity. However, it overestimated the DXA-calculated percent fat of children with obesity by 12% in boys and 6% in girls.76
Reliability can be strong with well-trained and skilled staff. In a large, international study assessing the precision of measuring skinfold thickness and circumferences to inform on fat distribution, the intra-observer technical error of measurements (TEMs) ranged between 0.12 and 0.47 mm for skinfold thickness (triceps, subscapular, biceps, iliac crest) and between 0.09 and 1.24 cm for circumference measurements. Intra-observer reliability was 97.7% for skinfold thickness (triceps, subscapular, biceps, iliac crest) and 94.7% for circumferences (neck, arm, waist, hip). Inter-observer TEMs ranged between 0.13 and 0.97 mm for skinfold thicknesses and between 0.18 and 1.01 cm for circumferences.77
Reference Data
National reference data for triceps and subscapular skinfold thicknesses are available from the NHANES 2007–2010 sample for infants and children 2 months to 19 years.72,78 These reference data are the most recent population-based reference data available for comparisons.
Accessibility, Training, and Costs
Skinfold equipment is accessible, highly portable, and relatively affordable. Cost of research grade calipers is incurred at time of purchase ($200 to $500), and little cost is incurred thereafter. Considerable expertise and training are necessary. Training must be conducted by a skilled technician to achieve high precision (low intra-observer variability). Whether these measurements are being collected at a single study location or across multiple study locations, it is imperative to standardize the methodology, as well as train and certify the participating staff to decrease measurement error.
Acceptability, Participant Burden, and Risk
Acceptability is high when privacy is maintained. The method is safe to conduct and carries little risk to participants. The method is considered noninvasive; however, some participants may experience slight discomfort during the procedure. It may be challenging to conduct in younger pediatric populations, as children are required to be calm and cooperative. Error may result from excessive movement.
Summary
Skinfold measurements are acceptable and feasible for use. They are safe, noninvasive, and relatively inexpensive to collect, but they require more significant training and skill for accurate and consistent measurement than do other methods. They are often used in large-scale studies.
Waist Circumference
Circumferences provide measurements that assess body size or dimensions at the specific region of the body that is measured. Waist or abdominal circumference provides information on central body fat distribution. It is generally conducted on individuals who are older than 8 years of age.
Procedure
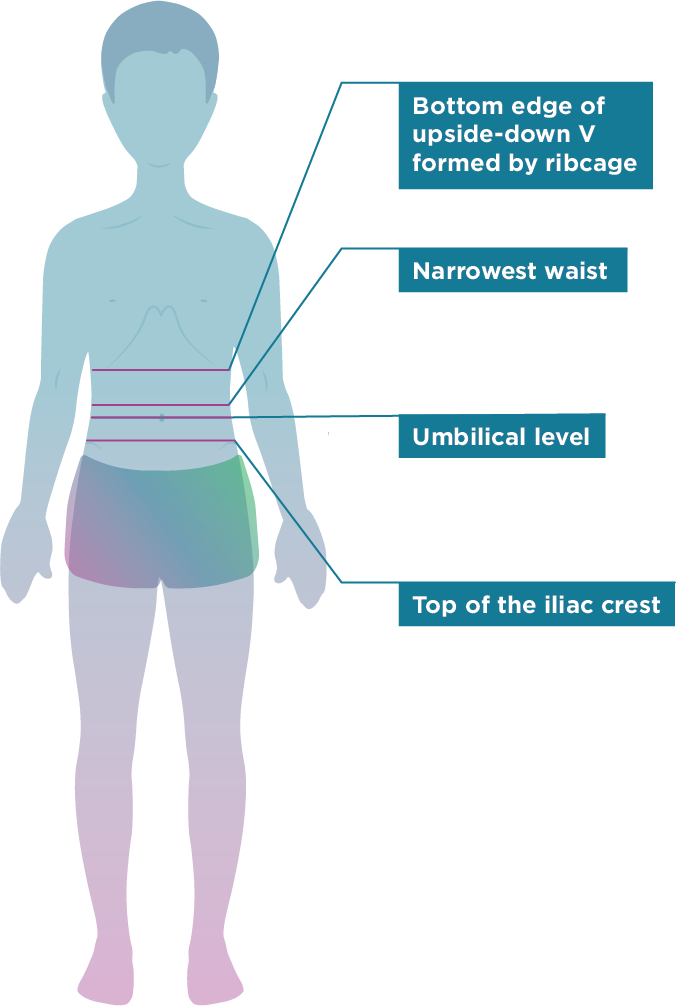
Figure 9: Commonly Measured Waist Circumference Sites
Waist circumference is measured using a measuring tape, preferably a tension-calibrated measuring tape. The participant must be wearing loose and movable clothing to allow for locating and measuring the correct site. Commonly measured sites that define the waist include (a) immediately below the lower most rib or the bottom edge of the upside-down V formed by the ribcage, (b) at the narrowest waist, (c) umbilical level, and (d) immediately above or top of the iliac crest (top border of the hip bone)79 (Figure 9). Two of these sites include a reference to at least one bony landmark. When lacking a bony landmark, waist circumference is measured at “the narrowest waist” based on visual inspection at the naval or umbilicus. Once the site is located, the tape is applied with minimal pressure against the skin so that the soft tissue is not compressed. The value of the measurement is recorded to the nearest 0.1 cm. The same location should be used consistently in a particular study protocol, and comparisons with other studies need to account for whether the location of the measurements were at the same location.
Estimates of Body Fat Distribution, Interpretation, and Limitations
Waist circumference is a commonly used surrogate measure of central fat distribution in adults. It may be a convenient approach to assess an unfavorable fat distribution in children as it correlates with visceral abdominal fat and with metabolic risk factors in children age 8 years and older. However, waist circumference reflects the sum of abdominal visceral and abdominal subcutaneous adipose tissue (VAT and SAT) and is unable to differentiate the quantity of one from the other. This shortcoming is evident in the fact that circumference measurements alone have a low sensitivity at young ages.80 Furthermore, growth-related changes in abdominal fat include changes in both VAT and SAT. Therefore, if VAT were to increase as SAT decreases, longitudinal waist circumference measurements might indicate no change thereby missing depot-specific changes. Acquiring longitudinal assessments during growth or when weight loss or weight gain occurs during interventions also may be difficult. The “narrowest waist” and level of the naval/umbilicus may change in anatomic location, and therefore follow-up measurements will not be acquired at the same location as baseline measurements. The location of these measurements is subjective and prone to greater measurement error, especially when measuring persons where a discernable “narrowest waist” is not visible, such as in persons with obesity.
Validity and Reliability
Moderate to high correlation exists for waist circumference with visceral fat in children depending on age.80 In newborns, waist circumference is a poor predictor of visceral adipose tissue compared to direct visualization methods such as MRI.81 Waist circumference measurements performed in triplicate at four sites for males and females (n = 93) aged 7–83 years have been shown to have high reproducibility and correlation with total body and trunk adiposity.79 Results from a meta-analysis of studies in children and youth aged 7–16 years found that although waist circumference accounted for 65% of the variance in visceral adipose tissue, ethnicity had an independent effect on the visceral adipose tissue-waist circumference relationship.80
A major limitation to the use of waist circumference as a methodology in children remains the fact that its use as a longitudinal assessment remains poorly described. Furthermore, the utility of waist circumference for different racial and ethnic groups and weight categories remains to be explored.
Reference Data
National reference data for waist circumference are available from the NHANES 2011-2014 NHANES sample for children aged 2–19 years.72 These reference data are the most recent population-based reference data available for comparisons.
Accessibility, Training, and Cost
Waist circumference equipment is highly accessible, portable, and low-cost. The cost of a spring-loaded tape measure is low (<$30). Tester training is required, but the level of skill is significantly less than that required for skinfold measurements. However, as children mature, the landmarks for determining the correct location to measure waist circumference may vary. High levels of central obesity may make it difficult to identify consistent landmarks for measuring waist circumference.
Acceptability, Participant Burden, and Risk
Acceptability is higher when privacy at time of measurement is maintained. The burden and risk are low, and the measure is noninvasive, but finding the locations for measuring waist circumference may cause significant uneasiness and may feel intrusive or embarrassing to the participant.
Summary
Waist circumference is a relatively quick, safe, and noninvasive surrogate method for assessing central body fat. It is inexpensive to collect but requires some training and skill in the accurate and consistent location of the site for measurement. It is appealing for large-scale studies, but issues with privacy and embarrassment may make it less feasible than previously described methods.