Section
4
Clinical Utility of Assessing Adiposity in Children
Clinical utility refers to the ability of the results of a measure to accurately identify children at risk of specific health outcomes to inform clinical decision-making in meaningful ways, such as guiding prevention and treatment efforts that can lead to improved health outcomes.
Ultimately, the utility of assessing childhood adiposity in research, clinical, and public health practice is driven by this goal, with research providing the evidence base for the use of the measure in practice.
Numerous adverse health outcomes have been shown to be associated with obesity in children, providing strong support for the potential value of measuring adiposity and intervening in children43,44 (Figure 2).
Figure 2: Adverse Childhood Obesity Health Outcomes
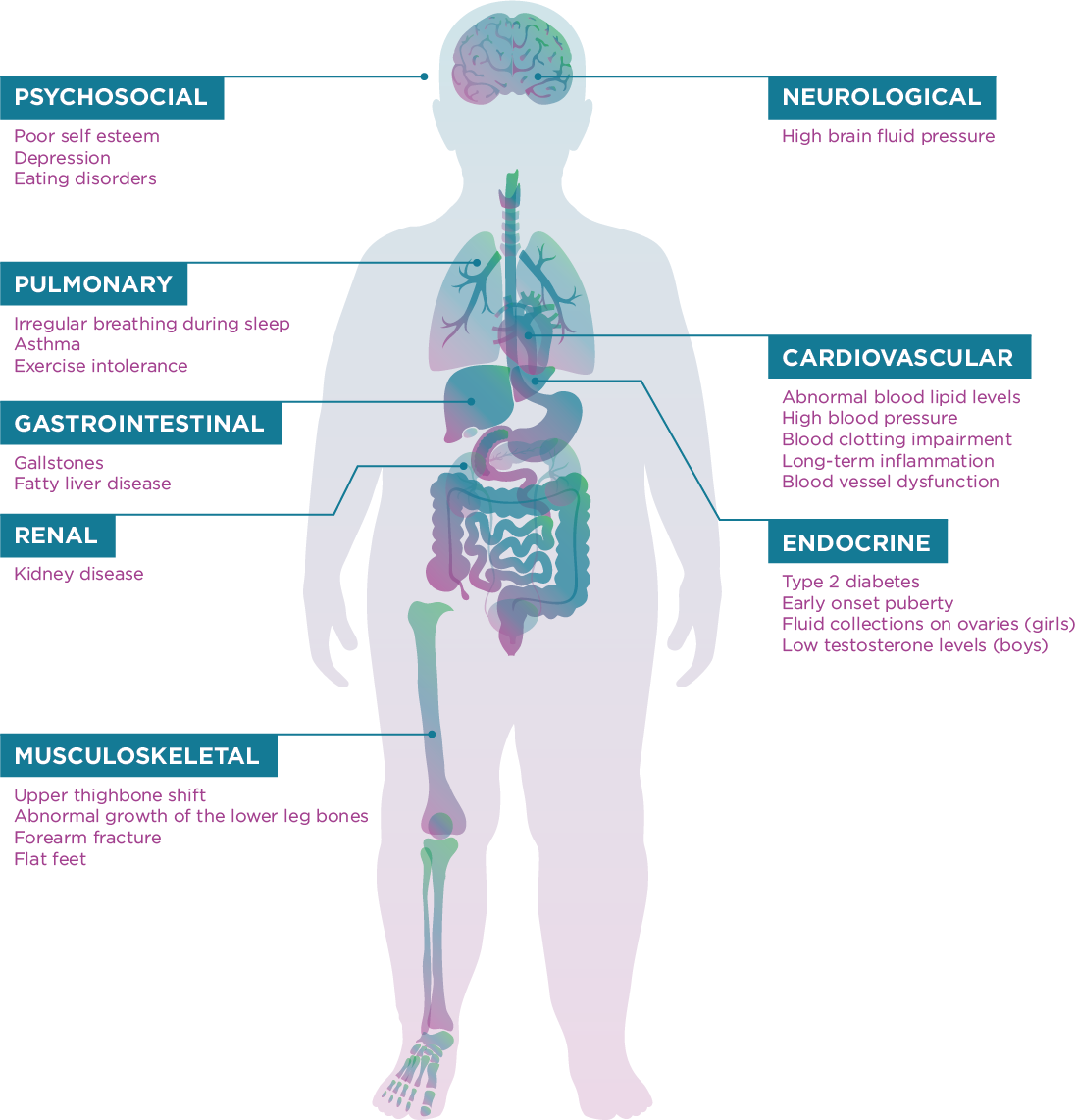
Childhood obesity has been associated with the development of hypertension, dyslipidemia, insulin resistance, type 2 diabetes, and fatty liver disease. Furthermore, a strong association exists between childhood obesity and developing adult cardiovascular risk factors levels, including blood pressure, triglycerides, and HDL cholesterol,45 as well as having obesity in adulthood.46 Negative psychological consequences of childhood obesity also are well-established. Weight stigma, primarily expressed as weight-based victimization, teasing, and bullying, can contribute to behaviors such as binge eating, social isolation, avoidance of health care services, decreased physical activity, and increased weight gain over time, which may worsen obesity and create barriers to healthy behavior change.47 Health care providers may exhibit weight bias and stigmatizing behaviors that include use of inappropriate-sized medical equipment as well as negative attitudes, such as associating patients with obesity with being lazy, lacking self-control, and being less intelligent.48 This bias may adversely affect quality of care and prevent patients with obesity from seeking medical care.
Given the well-documented negative health consequences associated with obesity in children, the assessment of body fat in clinical and public health practice for the purposes of screening, evaluation, and implementation of effective prevention and treatment strategies can have a major impact on the health and well-being of children. Several agencies and organizations have developed guidelines for screening, evaluation, and treatment of children with obesity in various settings, including schools and clinics (see Box 1). These recommendations are beyond the scope of this guide, but Section 5 of this guide reviews various methods of assessing body composition in children and addresses their validity (accuracy) and feasibility for use in these settings. Both validity and feasibility are important factors to consider when determining their utility in research settings as well as clinical and public health practice.
Box 1: Examples of Expert Group Recommendations for Assessment, Prevention, and Treatment of Childhood Obesity
- American Academy of Pediatrics: Assessment of Child and Adolescent Overweight and Obesity (Pediatrics Supplement)
- American Association of Clinical Endocrinologists: Clinical Practice Guidelines
- American Psychological Association: Clinical Practice Guideline for Multicomponent Behavioral Treatment of Obesity and Overweight in Children and Adolescents: Current State of the Evidence and Research Needs from the Guideline Development Panel (GDP) for Obesity Treatment of the American Psychological Association (APA)
- CDC BMI Measurement in Schools
- Report of the Commission on Ending Childhood Obesity
- U.S. Preventive Services Task Force: Screening for Obesity in Children and Adolescents: Recommendation Statement